
Fibroids on The Uterus
Post Updated: January 11, 2022
This article is about my experience with fibroids on the uterus. And what I did to save my uterus.
Sometimes hysterectomies are unnecessary. There are other alternatives that could help in saving your uterus.
“Cis woman” is shorthand for “cisgender woman.” It defines a non-transgender woman.
Her assigned sex is female. And she still identifies with the gender culturally associated with her sex: woman.
To some it may be offensive. Yet, I do not mean any harm of offense. But I am proud to be a natural born woman
This means that when God created mankind from the dirt as the story says. God reproduced from that male a feminine counterpart.
Who was also mankind but with a womb, thus giving the origin of the name WOMAN? Womb man.
“God created human beings; he created them godlike, Reflecting God’s nature. He created them male and female.” (Genesis 1:27 MSG)
What makes me a woman is my womb, the original birthplace of my two children.
Thus, part of me holds a special connection to who I am and why I exist.
The health of my womb is important to me and should be important to every woman created who was born with a womb.
Which brings me to our topic fibroids on the uterus.
What Are Fibroids on The Uterus
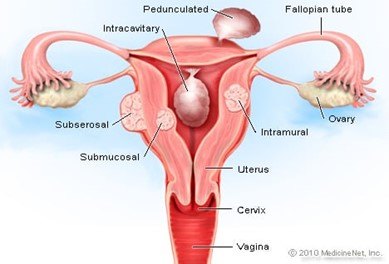
Uterine fibroids are a common type of noncancerous tumor that can grow in and on your uterus.
Not all fibroids cause symptoms, but when they do, symptoms can include heavy menstrual bleeding, back pain, frequent urination, and pain during sex.
What Is the Main Cause Of Fibroids On The Uterus?
Hormones. Estrogen and progesterone, two hormones that stimulate the development of the uterine lining during each menstrual cycle in preparation for pregnancy, appear to promote the growth of fibroids.
Fibroids contain more estrogen and progesterone receptors than typical uterine muscle cells do.
My Personal Journey with Fibroids on The Uterus
I sought my doctor after experiencing irregular blood flow during my periods. They were heavy and too long for my liking.
I wanted to know what was up. I like sex and at the time I was married (my husband has since passed away), so I needed to understand why my periods were staying around longer than usual.
As a woman, we are custom to having periods as part of life for us once we’ve become of age. Most females experience their menstrual cycles once a month from 3-8 days.
Menstrual cycles longer than this is abnormal. And torture for the woman going through this irregularity.
As a result of the irregular bleeding, I developed Amenia.
A condition marked by a deficiency of red blood cells. Of hemoglobin in the blood, resulting in paleness and fatigue.
My OB-GYN wanted to run a test to see what was causing the irregular bleeding.
The first test I had was an ultrasound to see if they saw anything in the uterus. They did! It appeared to be polyps.
Uterine polyps and Endometrial polyps are irregularities of the inner uterine lining. Something like fleshy skin tags, only on the inside.
Polyps are often the source of irregular bleeding and can be a large nuisance, BUT they are not cancerous.
Polyps of the uterine lining are often difficult to see on regular ultrasounds. But a “sono-hyst” (sonohysterography) or saline-infused ultrasound. Is much better at diagnosing this more.
The next test was an Endometrial Biopsy. According to the Mayo Clinic an endometrial biopsy. Is the removal of a small piece of tissue from the endometrium (the lining of the uterus).
This tissue sample can show cell changes due to abnormal tissues. Or variations in hormone levels.
Taking a small sample of endometrial tissue. Helps your doctor diagnose certain medical conditions.
She wanted to test the tissue from the uterus to ensure there was no cancer. Praise God there was no cancer.
She did a hormone test to check for imbalances. In which the hormones did not show any abnormalities.
We then discussed what was next. She wanted to get a better look at the polyps for quantity, size, and location.
She scheduled me for a saline-infused ultrasound. Which I stated is much better at accurately diagnosing polyps.
I had the procedure done. I was able to get a better look at the polyp. It appeared to be only one.
But that one polyp was wreaking havoc in my body. It had invaded my life like a squatter invades property that doesn’t belong to them.
After the procedure, she discussed treatment. The treatment she suggested was to have a hysteroscopy endometrial ablation.
Of course, I had never heard of it before. Usually when women have trouble with their uterus the first thing that I hear must be done is a hysterectomy.
The Cleveland Clinic reports that a hysterectomy is surgery. To remove a woman’s uterus (also known as the womb). The uterus is where a baby grows when a woman is pregnant.
During the surgery, the whole uterus is usually removed. Your doctor may also remove your fallopian tubes and ovaries.
After a hysterectomy, you no longer have menstrual periods and cannot become pregnant.
Hysterectomy is the second-most common significant operation. Performed on females inside the United States. The most common is cesarean section delivery.
Every year, more than 600,000 women undergo a hysterectomy. Some progressive doctors claim that up to 90% of hysterectomies are unnecessary.
More conservative estimates put that number between 20–30%.
Either way, that is a lot of women that may be having unnecessary hysterectomies.
I didn’t want that at all, and I wanted to avoid it at all costs. So, the doctor had my attention because she didn’t say Hysterectomy.
Why Are There So Many Hysterectomies?
There are quite a few reasons why women consider a hysterectomy.
The most common are intense bleeding. Large fibroids, endometrial polyps, endometriosis, causing debilitating pain and discomfort. And other endometrial concerns.
Some women have discomfort or bloating that accompanies a large fibroid uterus. They sometimes have uterine prolapse, (a condition in which the uterus drops).
More serious symptoms include cancers of the uterus or ovaries. Conditions that merit immediate surgery.
But if we take a closer look. The latter is uncommon and leaves women with few choices.
This conversation and topic are for women. Who is considering surgery for less clear-cut reasons.
Throughout traditional medical practices. Heavy blood loss is defined as “dysfunctional uterine bleeding”.
When it is not the normal amount of bleeding, but no demonstrable organic pathology. The diagnosis exclusion since organic pathology must always be ruled out.
What may be more useful for us to identify as “dysfunctional.” Or imbalanced. Are environmental and lifestyle influences. Affecting our hormones and sending the uterus mixed messages.

Every now and then these influences lead to a state of estrogen dominance. And in other cases, the menses may be out of sync, because of general hormonal imbalance.
In whichever the case. Tuning in and paying attention to what the body and mind need can restore balance.
Furthermore, what is dysfunctional for one woman may not be for another. And the term is somewhat subjective by nature. So, it should be with a knowledgeable and experienced provider.
Having reached a state of hormonal imbalance. A woman’s body can get stuck, and even her greatest efforts to restore balance can take quite a few months.
The annoyance of having to change pads hourly. Doubling up on tampons, washing extra linen, never wearing white at that time of the month. Or any light colors for that matter.
And timing activities around the heavy flow. Leads several women to the end of their reproductive rope.
When women in this situation ask for a hysterectomy. Most doctors in America will respond by scheduling surgery as soon as possible. Who can blame them?
But surgery should never be the first or even the second, recourse in the face of heavy bleeding.
I know plenty of people who have had hysterectomies. Most were because of heavy and irregular bleeding.

BACK TO MY PERSONAL STORY!
I wanted to save my uterus! I knew I didn’t want to have more babies.
I had already had two cesarean’s (c-sections) and I didn’t want to have another.
After discussion with my husband at the time, who already had plenty of children. From previous situation ships.
I was sure without a doubt I didn’t want to go through the process of pregnancy again.
Yet, I never said I wanted to give up my uterus. She is a part of me.
She’s part of my support system for my entire body. I didn’t want to know what life would be like without her.
The uterus is the nurturer and holds the creative force of life. It is the most creative and feminine one-of-a-kind female organ.
The uterus is the ONLY part of the female organ where there is no male counterpart.
Like the other parts of the female’s organs counterparts such as the vulva and the vagina.
Check Out This Fun Explainer Video. Talking About “The Girlfriends and Our Female Organs”
I found out I didn’t have to have a hysterectomy after all. I listened as she explained what a Hysteroscopy Endometrial Ablation consisted of.
She explained that the polyps were non-cancerous. I was not beginning or entering menopause yet.
My hormones showed no abnormalities, and the cause of the polyps was not known.
She also explained that the hysteroscopy would allow her to go into the uterus. Vacuum out the polyps but there was no guarantee that the polyps would not come back.
To prevent them from coming back the endometrial ablation. In layman terms mean the burning of the uterine lining.
The anemia would more than like stop because I would not bleed for as long as I was which would range from 7-14 days.
As she spoke. I wondered why were there so many women having their uteruses completely removed. For trivial matters when there are other alternatives.
So, I decided to research all the information on Hysteroscopy Endometrial Ablation.
It is two procedures performed at the same time. Which is slightly more invasive but less traumatic than a hysterectomy.
Below is everything you need to know about fibrosis of the uterus, hysterectomy, and hysteroscopy endometrial ablation.
UPDATE: Since I’ve had this procedure. I no longer have anemia. My periods are back normal. I just no longer have my wonderful husband to have amazing sex with again.

Love Below Intimates LLC
FAQs
What Is Fibroids on The Uterus?
Uterine fibroids are benign tumors that originate in the uterus (womb). These tumors are common and occur in about 20% to 80% of all women by the time they reach age 50. Fibroids are most common in women in their 40s and early 50s. Not all women with fibroids have symptoms.
What are The Symptoms of Fibroids?
Most fibroids do not cause any symptoms, but some women with fibroids can have:
- A feeling of fullness in the pelvic area (lower stomach area)
- Heavy bleeding (which can be heavy enough to cause anemia) or painful periods
- Enlargement of the lower abdomen
- Frequent urination
- Pain during sex
- Lower back pain
- Complications during pregnancy and labor, including a six-time greater risk of cesarean section
- Reproductive problems, such as infertility, which is very rare
What are The Causes of Fibroids in the Uterus?
It is not known exactly why women develop these tumors. There are some potential known causes. Researchers think that more than one factor could play a role. These factors could be:
- Hormonal (affected by estrogen and progesterone levels)
- Genetic (runs in families)
Family history is a key factor. Since there is often a history of fibroids developing in women of the same family. Race also appears to play a role.
Women of African descent are two to three times more likely to develop fibroids. Then women of other races.
Because no one knows for sure what causes fibroids, we also don’t know what causes them to grow or shrink.
Can Fibroids Cause Cancer?
Fibroids are almost always benign (not cancerous). Rarely (less than one in 1,000) a cancerous fibroid will occur. Having fibroids does not increase the risk of developing a cancerous fibroid. Having fibroids does not increase a woman’s chances of getting other forms of cancer. In the uterus.
What Is Hysteroscopy?
A Hysteroscopy is a procedure that allows your doctor to look inside your uterus. To diagnose and treat the causes of abnormal bleeding.
Hysteroscopy uses a hysteroscope. A thin, lighted tube is inserted into the vagina to examine the cervix and inside of the uterus. Hysteroscopy can be either diagnostic or operative.
What Is A Operative Hysteroscopy?
Operative hysteroscopy corrects an abnormal condition. That is detectable during a diagnostic hysteroscopy.
If an abnormal condition is detected during the diagnostic hysteroscopy. Operative hysteroscopy can often be at the same time, avoiding the need for a second surgery.
During operative hysteroscopy, small instruments are used to correct the condition. Are inserted through the hysteroscope.
When Is Operative Hysteroscopy Used?
Your doctor may perform hysteroscopy to correct the following uterine conditions:
- Polyps and fibroids. Hysteroscopy to remove these non-cancerous growths found in the uterus.
- Adhesions. Also known as Asherman’s Syndrome. Uterine adhesions are bands of scar tissue that can form in the uterus. It may lead to changes in menstrual flow as well as infertility. Hysteroscopy can help your doctor locate and remove the adhesions.
- Septum’s. Hysteroscopy can help determine whether you have a uterine septum. A malformation of the uterus that is present from birth.
- Abnormal bleeding. Hysteroscopy can help identify the cause of heavy or lengthy menstrual flow. As well as bleeding between periods or after menopause. Endometrial ablation is one procedure in which the hysteroscope. Along with other instruments. Is used to destroy the uterine lining to treat some causes of heavy bleeding.
What Are The Benefits Of A Hysteroscopy?
Compared with other, more invasive procedures, hysteroscopy may provide the following advantages:
How Safe Is Hysteroscopy?
Hysteroscopy is a safe procedure. But, as with any type of surgery, complications are possible.
Complications occur in less than 1 percent of cases and can include.
- Risks associated with anesthesia
- Infection
- Heavy bleeding
- Injury to the cervix, uterus, bowel, or bladder
- Intrauterine scarring
- Reaction to the substance used to expand the uterus
When Should The Procedure Be Performed?
Your doctor may recommend scheduling the hysteroscopy the first week after your menstrual.
This timing will provide the doctor with the best view of the inside of your uterus.
Hysteroscopy is also performed to determine the cause of unexplained bleeding. Or spotting in postmenopausal women.
The type of anesthesia used. Where the hysteroscopy is performed in a hospital or doctor’s office.
And whether other procedures are at the same time. Are important factors to consider.
In my case, I had to have general anesthesia. The numbing of the entire body for the entire time of the surgery.
My procedure was in a hospital as an outpatient. In certain circumstances.
Such as if your doctor is concerned about your reaction to anesthesia. It needs an overnight stay.
Once the doctor vacuums out the polyps. They will perform the second procedure which is an Endometrial Ablation.
What Is An Endometrial Ablation?
An Endometrial Ablation is a procedure that destroys (ablates). The lining of your uterus (endometrium).
The goal of endometrial ablation is to reduce menstrual flow. In some women, menstrual flow may stop completely.
No incisions are needed for endometrial ablation. Your doctor inserts slender tools. Through the passageway between your vagina and uterus (cervix). The tools vary, depending on the method used to ablate the endometrium.
They might include extreme cold, heated fluids, microwave energy, or high-energy radio frequencies. Factors such as the size and condition of your uterus.
It will help determine which endometrial ablation method is most appropriate.
Why Endometrial Ablation?
Endometrial ablation is a treatment for excessive menstrual blood loss. Your doctor might recommend endometrial ablation if you have.
- Heavy periods, sometimes defined as soaking a pad or tampon every two hours or less
- Bleeding that lasts longer than eight days
- Anemia from excessive blood loss
To reduce menstrual bleeding. Doctors generally start by prescribing medications or an intrauterine device (IUD).
Endometrial ablation might be an option if these other treatments don’t help. Or if you’re not able to have other therapies.
Endometrial ablation generally isn’t recommended for postmenopausal women or women who have:
- Certain abnormalities of the uterus
- Cancer of the uterus, or an increased risk of uterine cancer
- An active pelvic infection
What Are the Risks Of Endometrial Ablation?
Complications of endometrial ablation are rare and can include:
- Pain, bleeding, or infection
- Heat or cold damage to nearby organs
- A puncture injury of the uterine wall from surgical instruments
What About Future Fertility?
Pregnancy can occur after endometrial ablation. But these pregnancies might be a higher risk to mother and baby.
The pregnancy might end in miscarriage. Because the lining of the uterus has been damaged.
The pregnancy might occur in the fallopian tubes. Or cervix instead of the uterus (ectopic pregnancy).
Some types of sterilization procedures. Can be at the time of endometrial ablation.
If you are having an endometrial ablation. Long-lasting contraception or sterilization is recommended to prevent pregnancy.
What Happens After The Procedure?
After endometrial ablation, you might experience.
- Cramps. You may have menstrual-like cramps for a few days. Over-the-counter medications such as ibuprofen or acetaminophen can help relieve cramping.
- Vaginal discharge. A watery discharge, mixed with blood, may occur for a few weeks. The discharge is heaviest for the first few days after the procedure.
- Frequent urination. You may need to pass urine more often during the first 24 hours after endometrial ablation.
What Are The Results Of Endometrial Ablation?
It might take a few months to see the results. But endometrial ablation usually reduces the amount of blood lost during menstruation.
Most women will have lighter periods, and some will stop having periods. Endometrial ablation isn’t a sterilization procedure.
So, you should continue to use contraception if you are currently using it.
Pregnancy might still be possible, but it will likely be hazardous and end in miscarriage.
Although there are many benefits associated with Hysteroscopy Endometrial Ablation.
It may not be appropriate for some patients. A doctor who specializes in this procedure.
Will consult with your primary care physician. To determine whether it is appropriate for you.
I decided that this was the best method for me.
Take back the power of your body! You only get one body. You only get one uterus!
Use wisdom and knowledge to give it the best tender loving care possible.
I hope this article inspires you to appreciate your God-given body and do what is in your own best interest.
Be inspired! Be Healthy! Be Free to Live With Your Uterus!
What are your thoughts? Would you undergo hysteroscopy endometrial ablation?
Do you know someone who has had this procedure? Have you already undergone the procedure? If so, are you happy and comfortable with the results?
I would love to hear more insight from you! Please leave your comment in the form below.
Before you go would you be so kind and share this article on your social media page. With the hashtag #SaveTheUterus
Oh! Sign up for my email list.
Thank you in advance!



Thank you for the exposure of fibroids on the uterus. I am a man, so I do not understand these things. However, I believe it is important to understand these things to know what our loved ones are going through. I will definitely share this with my wife and see if she knows about fibriods and other stuff.
Thank you for stopping by Bernard! And thank you for sharing this with your wife!